Case Study | Disruptive Innovation in Lincolnshire System
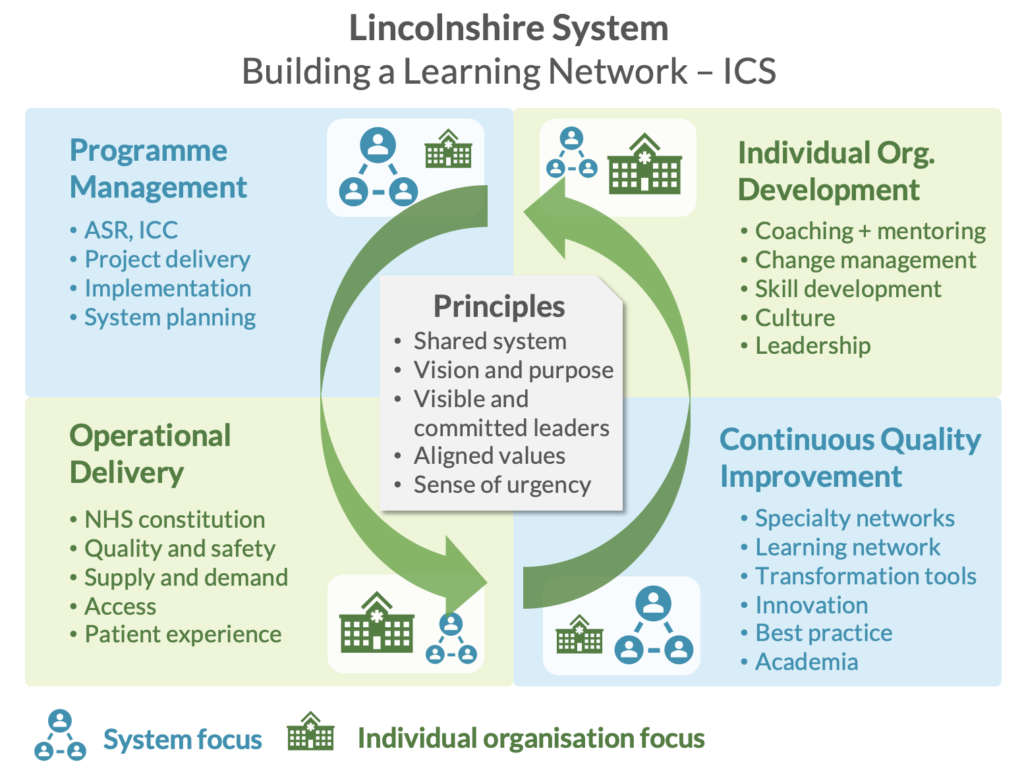
With the introduction of integrated care systems (ICSs) across the NHS, Lincolnshire System, which serves a population of over 800,000 people across a large geographical area, has been exploring how to create a delivery methodology for the system. All four key stakeholder NHS organizations have engaged in new people-driven change through disruptive innovation to create local change agents and a reinvigorated passion for continuous improvement.
Challenge
Lincolnshire had been facing long-standing quality, financial and workforce challenges. Dynamic systems face constant challenge and scrutiny, layered with multiple, conflicting priorities. With the transition towards integrated care systems and a move away from a competition/market economy, there was an opportunity to help the Lincolnshire system use the learning and additional sense of urgency from the COVID-19 crisis to establish a renewed appetite for disruptive innovation on its more enduring challenges.
Solution and approach
Our Institute experts facilitated three 10-week bespoke programs for 75 participants representing a range of roles from across the system. Leaders first learned about enabling behaviors, myth busting and establishing a system concord and team ethos. The improvement training program focused on action, acknowledging the systems and learnings already in place within Lincolnshire while exposing them to new process improvement tools and approaches, thus laying the foundation of a more robust learning system focused on continuous improvement with frontline team members taking action.
In early 2021, 11 people underwent the Advanced Process Improvement Training program to develop their capability and capacity even further and lead on successful change and service improvement to long-standing issues in their system. Through the design of the program, Lincolnshire System is building a dynamic learning network needed to establish the culture where frontline staff feel enabled to act and implement improvement. This work is creating a social movement and excitement for change. Each change agent is looking at their own area of work and demonstrating small acts of improvement every week, which exponentially multiply as more partners engage and collaborate within organizations and across the system.
Results from initial program
- IV iron therapy redesigned and standardized saving six weeks of ‘chair’ time (day case) and seven weeks of nursing time. Patients also have reduced visits. Next steps are to provide direct GP access thereby reducing outpatient referrals.
- Deep vein thrombosis ultrasound access standardized across United Lincolnshire Hospitals NHS Trust, meaning reduction in same day emergency care referrals (in Boston) and reduced wait from 10 days to 48 hours. Increase in capacity from 20 scans over five days to 30 scans over six days. This improves patient safety as patients are not on prophylactic anticoagulants whilst waiting for an ultrasound test. Next steps are to relaunch exiting LES in East GP practices and facilitate training and feedback sessions.
- Redesign of single liver pathway to seven standardized pathways with GP decision ‘tree’. This supports GP decision-making and care in primary care and more appropriate access to acute liver pathway and diagnostics. Next steps are to launch new pathways with facilitated training and feedback sessions for primary care.
- Advanced Process Improvement Training – 11 people from across the system were teamed up to apply the tools and techniques whilst teaching front-line staff and delivering improvements. This proved so successful, two GP practices invested £70K of their own money to continue the work in their primary care network.
“The outcome [of the advocate training] has been a renewed energy and enthusiasm to apply the tools and techniques to care pathways across the system which have already demonstrated significant benefit to patients and staff. Adopting the lean methodology is crucial to our pathway work with the patient at the centre and reflection on a culture of quality and safety.”
Jim Heys, Consultant, Lincolnshire Learning Network



