Eliminating Health Care Waste Improves Sepsis Recognition
Why waste elimination is essential to improving health care
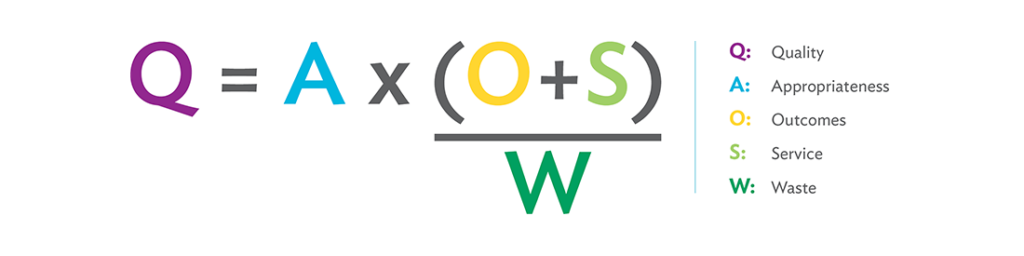
Waste elimination is essential to the Virginia Mason Production System (VMPS) and lean methodology. The waste in health care prevents health care teams from delivering the highest quality of care and service to patients. In the VMPS waste equation [shown below], waste is intentionally represented as a drain on quality in the denominator, where previously cost was represented.
The impacts of waste reach far beyond monetary effects. It consumes precious resources — people, time and material. In some clinical scenarios, this means the difference between life and death. An example is the frequent occurrence of patients who develop sepsis, which contributes to as many as half of all U.S. hospital deaths. From the latest research studies and national guidelines, we know that the early recognition, diagnosis and treatment of sepsis are key to saving thousands of lives each year and reducing the high costs of sepsis-related treatment. And we know that with sepsis, the waste of time due to defects, over-processing, hidden information, etc., directly correlates with patient outcomes. By removing waste and improving the process of identification and early treatment, providers can reduce the costly outcomes of care delivered too late and even save lives.
Waste elimination benefits any process. It’s important to remember that waste elimination is about process, not people, and it helps to reduce the burden of work and builds-in quality.
Waste elimination in action at Virginia Mason
At Virginia Mason the identification and elimination of waste as part of everyday work and through staff-generated ideas is a daily focus. It’s also important in the preparation for formal improvement events and as an actual measured process target. Reduction of waste is captured on target progress reports in terms of inventory, space, and lead time reductions. Virginia Mason has hundreds of examples of how focusing on waste has increased quality.
In one example, the sterile processing team worked with the neurosurgery team to use the lean methodology of 5S (sort, simplify, sweep, standardize and self-discipline) in their review of the laminectomy surgical case sets. Using data and stakeholder input, they reviewed the set contents, removed instruments no longer used, added items that were frequently provided ad hoc, and ensured that instruments for rare but emergent situations were still available. By tackling the waste of inventory, they reduced the laminectomy case set from 152 items down to 59 items per kit, a 61 percent decrease. They also arranged the instruments in the kit to match how they are set up in the OR, tackling the waste of motion and overprocessing. Furthermore, they reduced the waste of transportation by decreasing the number of sets full of unused instruments that staff members were delivering and retrieving, and they saved sterilizing time and resources because they weren’t reprocessing all these unused instruments. After the work with the laminectomy surgical sets, the team also applied 5S to the orthopedics and craniotomy surgical sets.
But not all waste elimination needs to be complicated or on a big scale. For example, a team member in the short-stay procedural area noticed that a large amount of partially used water bottles were being thrown away every day. At baseline, the department discovered they were spending over 12,000 dollars per year plus staff time to supply water bottles and disposal. So the team worked together, determined that they did not need to offer water bottles to patients, and implemented less wasteful options for hydration.
Virginia Mason has also made exciting gains in improving sepsis outcomes. The sepsis team saw that a waste of time (a delay in diagnosis and treatment) and defects (missed interventions) could cost sepsis patients their lives, so they began what would become a multiyear journey to improve sepsis outcomes. They focused relentlessly on the full value stream from early identification to completion of treatment, regardless of location — whether that was the emergency department, acute care unit or critical care unit. The team employed all of the VMPS methods with an intense focus on mistake-proofing, skill-task alignment and innovation to improve quality and reduce our overall sepsis mortality by 30 percent.
How getting rid of waste helped Virginia Mason make quicker diagnoses of sepsis
At baseline, the time to recognize a patient who developed sepsis during the course of hospitalization (versus reason for admission) was 8 hours due to delays in provider assessment, diagnosis and confirmatory lab values. The improvement team worked together to create the Sepsis Nurse Initiated Protocol, known as the “Sepsis Power Hour,” which gave nurses the authority and tools needed to quickly initiate evidence-based sepsis treatment. The protocol triggers, based on standardized nursing-observed changes in a patient’s condition, provided critical setup for provider decision making. This work built on previous improvement efforts, including the rapid identification of sepsis when a patient presented to the emergency department and a reframing of the protocol that the diagnosis and treatment depended on the presence of the physician. Implementation of the Power Hour reduced inpatient sepsis recognition time from 8 hours — all the way down to 30 minutes. In addition to quicker identification, the Power Hour supported compliance with defined best practices or bundle elements. Based on a review of Power Hours completed between July 2014 and February 2015, 75 percent of patients received specific bundle elements within one hour, compared to only 32 percent of regular care patients for the same elements.
Other improvements targeting waste in the sepsis value stream included a new evidence-based order set, point-of-care lactic acid test, and the stocking of common sepsis antibiotics in the emergency department, which eliminated significant wait time for delivery.
The improvement team worked together to create the Sepsis Nurse Initiated Protocol, known as the ‘Sepsis Power Hour,’ which gave nurses the authority and tools needed to quickly initiate evidence-based sepsis treatment. The protocol triggers, based on standardized nursing-observed changes in patient condition, provided critical setup for provider decision making.
Additional measures taken
Initial process improvement work mainly supported treating severe sepsis, yet because studies showed that earlier detection and treatment led to better patient outcomes, specifically after deploying therapy bundles within three hours, Virginia Mason formed the Sepsis Advisory Group, charging its members to do what had seemed undoable — early recognition, diagnosis and treatment in one hour. The group, made up of physicians, nurses, Kaizen Promotion Office team members, and specialists in pharmacy, infectious disease, and clinical practice and professional development, orchestrated a series of aggressive formal improvement events. They have also delivered extensive training on the nurse-initiated protocol and frontline-staff sepsis response drills.
Virginia Mason intentionally integrated the patient voice and experience into this work through formal experience-based design (EBD) methods, such as interviews with patients and families who survived sepsis, and the inclusion of patient and family volunteers on formal improvement events. Hearing patients share their experiences, in their own words, truly underscored the tremendous human cost of sepsis and inspired future improvement work.
After significant gains for patients, looking ahead
The vision for sepsis care includes a continued focus on bundle compliance and mortality reduction. The team is also analyzing and reducing hospital readmissions after a sepsis diagnosis, expanding sepsis practices across the care continuum, and further engaging patients and their families.
Since implementing the Sepsis Power Hour protocol, Virginia Mason has achieved impressive improvement metrics:
- The average 90-day sepsis episode cost at Virginia Mason is $22,082, compared to the national average of $28,130 – a savings of 21% per episode
- Virginia Mason has experienced a 15% reduction in discharges to long-term care facilities
- Rapid response calls were reduced by 66%, from 120 calls per month to 40
- An 80% success rate was achieved delivering the bundle in under one hour
As sepsis care results improve, the team will seek to share knowledge and innovations with partner organizations, including members of the High Value Healthcare Collaborative and professional associations. Bringing life-saving sepsis innovations to light is another prominent milestone in Virginia Mason’s journey to transform health care.





