Case Study | How Foundation Health Partners is Connecting Vision, Technology and a Structured Management Method to Accelerate Improvements
Foundation Health Partners’ vision is to become a patient-centered integrated health system that provides excellent care. Their ambitious approach includes creating a comprehensive strategic plan, implementing CareOps technology, and, in partnership with the Virginia Mason Institute, creating FHP Forward: their own comprehensive management system that provides tools, methods, and principles on the “how” related to achieving their vision.
“Everyone’s thinking about the power of new technology,” said Robbi Bishop, Executive Partner for Transformation Services at Virginia Mason Institute, “but what impact does the tech have on how your people work as they serve your community? What do you do with all that data? That’s where a robust improvement approach comes in.”
Over the past year and a half, Foundation Health Partners (FHP) has worked closely with VMI and Stat, their CareOps technology provider, to drive improvements in ambulatory care. The cumulative impact of investing in strategy, technology, and FHP Forward simultaneously has accelerated impact and improvement far beyond what any of those elements could achieve independently.
“This experience has been really magical in terms of changing mindsets,” said Dr. Angelique Ramirez, Chief Quality & Transformation Officer at FHP. “We started with a traditional mindset of scarcity: not enough staff, not enough time, not enough space. But through this transformative work, through being able to actually know where everyone is in real time, we have realized: we actually do have enough.”
“You really need all three ingredients to have strong results,” said Bishop, who noted that even in just the first year of this effort FHP saw better throughput, improvements in patient wait times and tangible impacts on team engagement.
About a year ago, the Fairbanks based healthcare system began developing FHP Forward, their management system rooted in the process improvement principles of the Virginia Mason Institute. At about the same time, they began to implement Stat, a digital care operations platform that promised to provide insight into patient wait times, provider movements, and more. The synchronous timing of these two endeavors has proved to be a perfect match. “It was perfect timing,” said Ian Petersen, VP for Customer Success at Stat, “Implementing Stat just as VMI’s process improvement workshops were happening meant that the team knew exactly what to do with the massive influx of real-time data.”
Seeing the Big Picture – and the Details
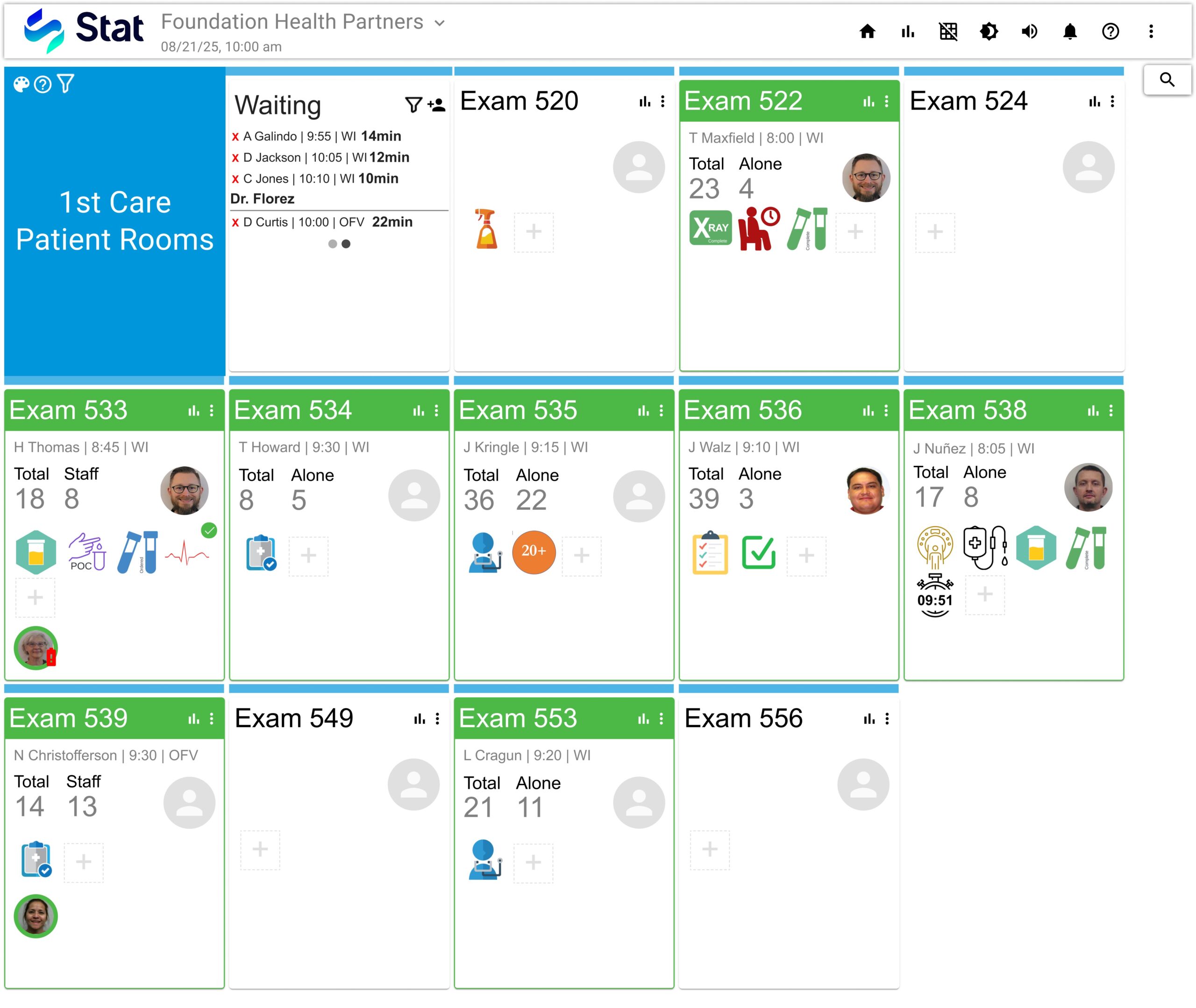
The Stat system is tailored to each clinic, but at a high level it offers a bird’s eye view into the status of every patient room and every patient currently being served. A single screen might display each room with its status, and if it’s occupied, the patient’s status as well such as waiting for labs, ready for provider, ready for discharge, etc. Each provider and staff member wears a badge that tracks their movements. There’s no need to search for a colleague in an office or in the nurse’s station, the location of everyone on shift can also be made visible. That visibility can have a major impact on so many of the Seven Wastes – especially Processing, Time, Motion, and Transportation. As Dr. Ramirez put it, “If someone’s not there when you need them, it can be easy to assume they’re not available.”
Room Lock
“We used to run into room lock all the time,” said Dr. Ramirez, referring to a situation where new patients can’t be checked in due to a lack of available rooms. “We knew we just needed more space to be able to serve all of our patients efficiently.” After the clinic implemented Stat in conjunction with their work on process improvement, room lock became a thing of the past. “At first, we thought we were just learning to improve our flow,” said Dr. Ramirez. “We saw lots of interesting new data. Then suddenly we realized: we never had a room lock!”
Dr. Ramirez explained that sometimes room lock had actually arisen out of the team’s desire to improve patient visit times. A provider would finish seeing a patient and discharge them directly to save time for the rest of the staff. But, others did not realize the discharge had happened and assumed that the room was still occupied, leaving patient rooms empty and stacking up longer wait times. “Everybody wants the right thing,” said Dr. Ramirez. “They just don’t know what the gaps are, and how what they’re doing might actually be making things harder for others.”
It was the merging of that collaborative instinct embedded into FHP Forward along with the real-time visibility from Stat’s that allowed the team to work seamlessly together to manage rooms and realize we actually do have enough space to serve our patients. In the clinic, just addressing the room lock problem reduced waiting room wait times by 26%.
Managing Data Overwhelm
For Jennifer Carlson, FHP Director, Ambulatory Care, having visibility into every patient’s status and wait times is a game changer. She described the previous system: a whiteboard with a system of circles and x’s and tick marks. According to Carlson, “It worked, but you never really understood how long a patient was waiting.” But the massive amount of data that opened up after implementing Stat could sometimes be overwhelming. Providers could limit their screens just to their rooms, and it gave them immediate actionable info: “‘Oh, Patient Jones is still in X-ray, to keep in flow I can go see another person while they’re away.’” But for staff the realization was a little slower. She says the big aha moment came one day when the internet went out and they had to go back to using the old white board with its circles and check marks. The contrast was a dramatic demonstration of the powerful transformation that had already taken root. Everyone was eager to get back online.
Data and Quality Improvement: A Transformative Partnership
For FHP, developing FHP Forward alongside Stat has been a virtuous cycle. To improve processes and reduce waste, we need to better understand the current state through observations and data – lots and lots of data. But data on its own can’t offer insight into what to do. The data offered by Stat provides critical insight needed to inform process improvement. From simple changes like knowing when a patient has been roomed to the profound realization that ‘room lock’ could be eliminated, this first year of FHP Forward and Stat has kicked off a new culture of improvement at FHP.
Dr. Ramirez is looking forward to continuing this work. “It’s all about our community, the patients, and doing the right thing.”
Why train with Virginia Mason Institute?
- Immediate results — Our training programs focus on creating immediate results while supporting broader changes that systematize and sustain learning and improvement.
- Personalized coaching — 1-on-1 virtual coaching and feedback helps students apply new tools in real time.
- Intimate cohorts emphasize peer-to-peer learning — Small cohorts in a virtual setting spark group interaction and expand networking opportunities.



