Case Study | A GP Practice Shows How the NHS Can Improve Patient Access
At a Glance
The Organization
Lincolnshire is a large rural county on the eastern coast of England. It contains 86 general practitioner (GP) groups and three National Health Service (NHS) trusts, which provide acute care, community care, and mental health care.
East Lindsey Medical Group is a GP practice in Lincolnshire with a staff of 70 serving roughly 14,000 patients.
Key Decisions
- Participating in leadership and process-improvement training focused on patient needs and staff empowerment
- Hiring an improvement director to oversee a new management system at East Lindsey Medical Group
- Creating an improvement board, including patient representatives, to evaluate priorities and progress
- Empowering front-line workers at the practice to improve reception, coding, and other processes related to patient access
Key Results
- Coding backlog at East Lindsey Medical Group reduced from 5,000 patient records to 0
- Reception team more engaged after redefining their role with new duties, training, and sense of purpose
- Staff turnover reduced to almost 0
The Context
Backlogs are crushing the NHS, and GPs are key to releasing the pressure
The number of patients waiting for care by the NHS is a critical matter in British healthcare today. Analysis by the British Medical Association shows that, as a result of pandemic-related disruptions and other factors, more than 7 million patients were waiting for services in January 2023. Five percent of those patients had been waiting for more than a year.
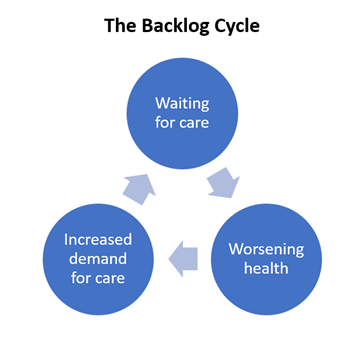
This patient backlog feeds a vicious cycle: Delaying care makes people sicker, which raises demand for urgent care, which creates more delays, which makes people sicker, and so on.
If the demand for care in England is a flood, then GP practices can act like trees planted upstream — capturing as much water as they can so that the runoff flowing to urgent care and hospitals is more manageable.
In order to do that, GPs must address their own patient access challenges.
“Throughout our careers, we value the concept of getting the patient to the right clinician at the right place at the right time. But I’m not sure we’ve ever really spent time thinking about or understanding what that statement actually means.”
— Dr. Neal Parkes, senior GP at East Lindsey Medical Group
The Challenge
“I’m sorry, I have no appointments to offer you”
By the mid 2010s, providers in Lincolnshire were struggling on multiple fronts. Regulators imposed reforms on the county’s acute hospital trust because of poor performance in both finance and quality.
GP practices struggled as well. At the East Lindsey Medical Group, too many calls came in for reception staff to handle. For those that were answered, there was only bad news.
“Morale was low on both ends of the phone. It’s hard to be told you have to wait weeks to see your doctor, but it’s also hard to deliver that message,” says Neal Parkes, M.D., senior GP at the practice.
The practice also wrestled with delays after a patient’s visit, with the team responsible for medical coding and scanning. In truth, there was no dedicated team, but rather 12 people with several other duties who made time for coding whenever they could fit it in. As a result, a backlog of 5,000 patient records sat uncoded and waiting each day.
The Solution
Senior GP brings home a new management system
To improve care throughout Lincolnshire, the local trusts enrolled 75 of the county’s healthcare leaders in a 10-week leadership training course with Virginia Mason Institute. Dr. Parkes was one of them, and he joined 10 other leaders for further training in process improvement, which included heavy doses of practical “field work.”
The trainings opened Dr. Parkes’ eyes to the many roles and processes that are instrumental in providing patients with the experience they expect and deserve.
“For me, the epiphany was that I probably have a very small role to play in the overall production line,” he says.
So he reframed his practice around identifying and honoring his patients’ actual needs and empowering his staff to satisfy them.
To lead that effort, he hired Maria Wilde, an improvement professional he met at the process improvement training. They created an improvement board to set priorities and discuss progress.
The improvement board includes three patient representatives who, in addition to their experience receiving care, have professional experience in areas like operational management. They also showed a strong interest in how the practice functions.
“It’s quite a challenging group, but that’s the point. To be challenging in a positive, constructive way,” says Wilde.
Wilde used a variety of methods she learned in her advanced training with the Institute to tackle the clinics’ challenges with access and backlogs. To address phone traffic and appointment availability, reception staff were tasked with documenting why patients were calling in. Receptionists were free to categorize calls in ways that made sense to them — with surprising results.
“They categorized demand in a very different way than I would, as a clinician, but also a very constructive way. Because they reflected more of the patient’s view of our services — this person needs a sick note, this one had a urinary tract infection,” Dr. Parkes recalls.
The practice also adopted a new phone service that gives receptionists better visibility into schedules and automatically informs callers when same-day appointments are full. A patient on the improvement board helped find the new service, which is less expensive than the previous one, despite fees from the outgoing phone vendor.
To help with coding, staff had initially demanded more team members, but the solution ended up being the opposite. Of the 12 team members who had previously shared coding duties, Wilde created a discrete team of five.
Then Wilde led the new team through a multi-day workshop to design a new process. The new process met the practice’s daily demand for coding — but there was still the problem of the 5,000-file backlog. The team worked overtime to bring it down, and they were done after two weeks.
“They absolutely blitzed the backlog,” says Wilde.
Driving change from the bottom up
Through the Institute’s training, Dr. Parkes realized that his role is to enable change, while the responsibility of enacting change falls to his staff. A similar dynamic applies to the wider landscape. Leaders at the top of the Lincolnshire system enabled GPs like Dr. Parkes to enact new ways of working in their clinics. These changes then have the chance to spread throughout the system, one clinic at a time.
This “bottom-up” dynamic is exactly how Virginia Mason Franciscan Health achieved its transformation. It didn’t happen all at once, and it wasn’t micromanaged from above. Rather, change spread slowly, as individual teams and clinics mastered different aspects of the new management system and passed their improvements on to others.
The primary care clinic in the city of Kirkland was an early catalyst, using the new system to tackle many of the same challenges faced by Dr. Parkes’ practice. Kirkland’s success with phone traffic and same-day appointments helped boost patient and staff satisfaction, restore it to financial health, and serve as a model for the rest of the organization.
Dr. Parkes would love to have the same effect in Lincolnshire.
“We hope to demonstrate that these methods really work, so other practices will notice and want some of what we’re having,” he says.
The Results
Backlogs reduced and staff regained their “mojo”
The coding team now processes 400-600 records per day and generally operates with zero backlog. The team falls behind occasionally, but now they escalate their work when the backlog reaches a few hundred, rather than a few thousand.
Over at reception, the team is inspired by a new view of their role: They’re not just answering phones — they’re performing triage and serving as care consultants. This has led to new qualifications, training, and opportunities for career progression.
“It’s incredibly powerful, because now this is a job they’re much more excited about doing,” says Dr. Parkes.
Staff turnover has been reduced to nearly zero. The only employee to leave in the last year did so to be closer to family.
Overall, Dr. Parkes sees his staff have got their “mojo” back.
“There’s more of a belief that we can change and make it better — for ourselves and for our patients,” he says
Why Partner with Virginia Mason Institute?
- Experience — The Institute has spent over 14 years helping NHS organizations large and small transform the way they work, based on the management system at Virginia Mason Francsiscan Health and our ongoing learning from working across 26 countries with independent validation.
- Practicality — We work alongside your teams to help build their internal capability, apply improvement tools, and deliver real-world change, in a psychologically safe environment that promotes learning and is free of blame
- Customization — We tailor our training and coaching to each organization and encourage leaders to take what they learn and make it their own — just as Dr. Parkes and Maria Wilde have done
Why train with Virginia Mason Institute?
- Immediate results — Our training programs focus on creating immediate results while supporting broader changes that systematize and sustain learning and improvement.
- Personalized coaching — 1-on-1 virtual coaching and feedback helps students apply new tools in real time.
- Intimate cohorts emphasize peer-to-peer learning — Small cohorts in a virtual setting spark group interaction and expand networking opportunities.