Case Study | Bringing Impact Within Reach
How hospitals, practices and leaders can implement NHS Impact
NHS Impact provides the blueprint for organisations throughout the system to
create lasting solutions to their most painful challenges. It consists of five core components based on time-tested improvement strategies used by leading healthcare organisations around the world.
But bringing the blueprint to life is a big job, and many in the NHS are unsure how to approach it.
The Virginia Mason Institute has partnered with organisations of all sizes, in more
than 20 countries, to develop the components that comprise NHS Impact. The insights below offer a glimpse of how leaders, teams and organisations like yours have used these components to reduce backlogs, reverse burnout, and provide the quality of care they aspire to for their patients.
Building a shared purpose and vision
In the past, the NHS has attempted to set a vision for the whole system. But it’s been hard for organisations to translate these broad campaigns to changes in daily work and to keep up with target metrics that change every year or two.
NHS Impact is different because it tasks organisations with establishing their own vision. This is a powerful opportunity for leaders to unite staff behind clear, consistent goals that are meaningful to the organisation. But for those who haven’t done it before, it can be overwhelming.
How they did it: Finding “true north” at a 218-bed community hospital
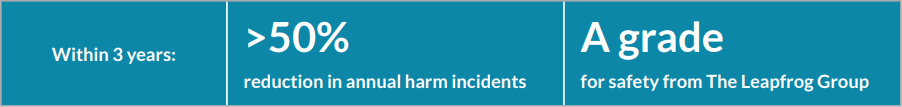
After a lab error at the University of Maryland St. Joseph Medical Center (UM SJMC) adversely affected two patients, executives committed to a new vision focused on patient safety.
To add clarity and accountability to the vision, the Virginia Mason Institute led executives through a meticulous process of setting goals and key metrics. Executives called these their “true north” and communicated them to individual departments and teams, who had autonomy to choose local areas of improvement that support the broader goals. This gave frontline workers a legitimate role in the organisation’s vision and, therefore, a substantial sense of purpose and ownership over it.
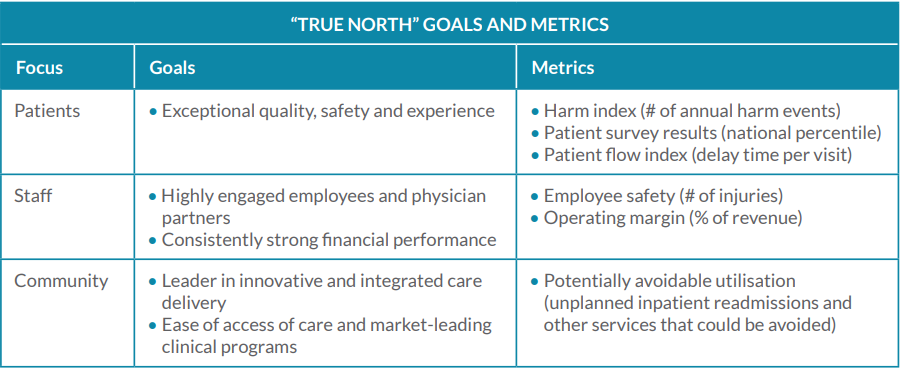
Guided by their true north, UM SJMC launched a new management system (including all components of NHS Impact) and achieved remarkable results.
Investing in people and culture
The unofficial culture at the NHS has long been characterised by command and control. System leaders rightly recognise that this has served staff and patients poorly, by stifling proactivity and inhibiting change. A new culture, grounded in listening and respect, is necessary for workers to thrive and improvement to flourish.
But culture change is not a simple exercise. It requires full commitment from leaders and a dedicated effort to not only identify new behaviours but also put them into daily practice.
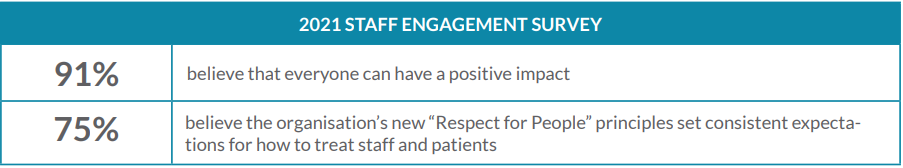
How they did it: Maintaining morale during the hardest year in healthcare
UW Health struggled with inconsistent values and communication norms across
the 17,000 employees and multiple hospitals that comprise the organisation. This
fed high turnover and a sense of futility among staff.
With the Virginia Mason Institute’s help, UW Health defined a clear and consistent
culture through a platform it called Respect for People. The platform houses five
high-level commitments, along with specific examples and strategies for how staff
can execute each one.
To ensure their new culture took root, the organisation:
- Provided introductory training to the entire staff
- Created a suite of digital tools and training modules for leaders to share with their teams
- Integrated Respect for People behaviours into annual goal setting and performance evaluations for
all employees
All this occurred amid the hailstorm of COVID-19, yet staff surveys showed engagement increased.
Developing leadership behaviours
Leaders at hospitals and across communities may feel especially trapped by “command and control.” Their early careers were shaped by it. Succeeding in their present positions may seem to depend on accepting control from above and exercising it on people below.
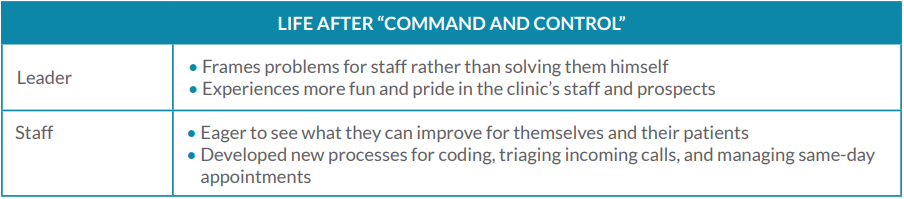
But in our experience, change is not only possible among leaders — it comes as a great relief. They feel better when they spend more time listening and empowering than dictating and disciplining. They have more time for the responsibilities they prefer to focus on. And their teams prove more productive, proactive and engaged.
How they did it: Enabling change in a GP practice
Staff at East Lindsey Medical Group, a series of GP practices across Lincolnshire county, were burnt out by the COVID-19 pandemic and the daily struggle to meet community demand. To help revitalise the clinic, Senior GP Dr Neal Parkes attended leadership training with the Virginia Mason Institute, followed by advanced training in process improvement.
The training opened Dr Parkes’ eyes to all the job tasks outside of his own that affect patients’ overall experience.
“I have a very important part to play in my bubble, but around me, allowing me to do what I do, is a huge production line.”
— Dr. Neal Parkes
This realisation led him to concentrate on enabling change, whilst allowing his staff to be the ones who drive it. Since changing his behaviour, Dr Parkes has witnessed numerous benefits in clinic operations and morale, with the team able to finish their shifts on time for the first time in years.
Building improvement capability and capacity
Many organisations in the NHS already have methods for improvement but struggle with knowing what to fix and whether a fix is working. The improvement capability and capacity envisioned by NHS Impact is not meant to replace existing methods, but rather enhance them with reliable ways of delineating problems and root causes, rapidly iterating on solutions, and measuring their effectiveness in the short and long term.
How they did it: Breaking down backlogs at an NHS trust
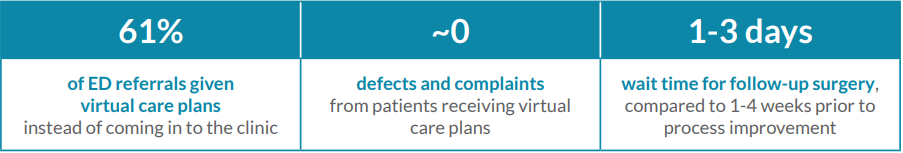
Dr Murali Bhat and his team at the fracture clinic in the Surrey and Sussex Healthcare NHS Trust (SASH)
struggled with 1,000 monthly emergency department (ED) referrals, causing long appointment delays, a crowded wait room and a growing elective surgery backlog.
Through leadership training with the Virginia Mason Institute, Dr Bhat learned tactics for analysing demand that led to a game-changing discovery: Most of the clinic’s patients could get their needs met without in-person appointments. Their follow-up care was straightforward based on data captured in the ED.
Dr Bhat and his colleagues created virtual care plans and a new process for screening referrals to see which patients actually needed in-person appointments. The new process cleared so much time on the appointment calendar that the clinic invited local primary care practices to send their urgent referrals through the emergency channel, rather than adding them to the elective backlog, as they did before.
Embedding improvement into management systems and processes
Combining all these components into a single management system takes time and effort. Leaders may view this work as separate from and even competing with their other priorities, but it’s not. In fact, it’s the only proven way to enable the breakthroughs in value and experience that leaders, staff and patients are looking for.
How they did it: Powering improvement across the U.K.
When the incoming CEO at Leeds Teaching Hospitals NHS Trust (Leeds) asked staff what their organisation’s top challenge was, the response was unambiguous: culture. So the trust got to work, gathering more input from staff to inform a definitive set of core values and behaviours.
Upon this cultural foundation, the Virginia Mason Institute helped Leeds build and combine the other
components of a complete management system. With a shared vision, healthy culture, new leadership style, and optimised methods of improvement, the trust utterly transformed its standing in finance, quality and staff engagement
“… the trust overall has moved in terms of the absolute measures from a £100m deficit to a £19m surplus, from a position of poor quality through requires improvement to good CQC, from one of the worst staff surveys to one of the best.”
— CEO, Leeds Teaching Hospitals NHS Trust
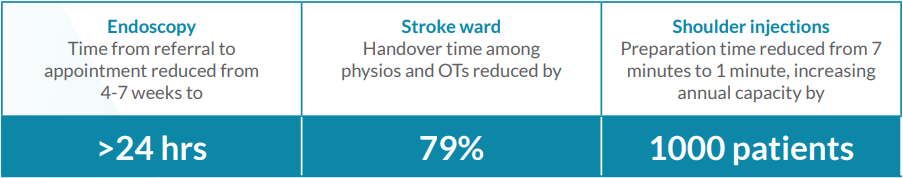
Similarly, at SASH, the leadership training provided to Dr Bhat and others was part of a larger collaboration with the Virginia Mason Institute to build an overarching management system. There, the new system has helped raise the trust’s CQC rating from Good to Outstanding and lower the time required for important care and services, including:
Blueprint for success
Reducing backlogs and waste and improving quality and morale starts with implementing NHS Impact. The five components enable a better future for the system, its workforce and its patients.
Wondering where and how to start? Taking that first step is always the hardest! The Virginia Mason Institute has helped clients at more than 200 sites worldwide take the necessary steps and ultimately become self-sufficient in sustaining a culture of continuous improvement across their organisations.
Contact us to learn where your journey might begin.
Why train with Virginia Mason Institute?
- Immediate results — Our training programs focus on creating immediate results while supporting broader changes that systematize and sustain learning and improvement.
- Personalized coaching — 1-on-1 virtual coaching and feedback helps students apply new tools in real time.
- Intimate cohorts emphasize peer-to-peer learning — Small cohorts in a virtual setting spark group interaction and expand networking opportunities.