Improving Team Well-Being: Addressing Provider Burnout with Culture and a Systems Approach
Burnout continues to be a leading challenge in healthcare. It can jeopardize patient experience and even quality and safety. Research has found that burnout among healthcare providers increases surgical errors, infection transmission and patient mortality.1
In 2021, healthcare systems are still recovering from the shock of pandemic-related changes. That shock will have ripple effects in the form of provider burnout. In a recent survey by the Kaiser Family Foundation, 3 in 10 healthcare workers said they are considering leaving the profession.
Fortunately, burnout is a solvable problem. It stems from stressors and patterns with deep roots in the ways that organizations and teams work. When you address those roots — by embracing principles of respect and improvement — the factors that used to cause staff to burn out instead can help them become more engaged and empowered.
What is burnout?
Burnout is the state we reach when we’re chronically exposed to stress. Workers who are burned out tend to feel exhausted, cynical and disconnected from their work. They may also lack empathy and a sense of personal accomplishment.2,3
This state arises from a combination of personal and external factors, including company culture and the nature of specific jobs or tasks. In a highly regulated and high-stakes profession like healthcare, these factors can be especially powerful.
According to the National Academy of Medicine (NAM), which studied the subject in a 2019 report, common causes and predictors of clinician burnout include:
- Long hours and overburden of work
- Time-consuming bureaucratic tasks
- Lack of respect in the workplace
- Lack of autonomy with work
Many organizations try to address burnout at the individual level — offering rewards or an occasional pizza lunch. But when you look at burnout’s true causes, you can see why interventions like these fall short: Someone who lacks autonomy in their job is no better off after a free lunch.
Burnout arises from systemic problems. To address it effectively, organizations have to make systemic changes.
COVID and Burnout: The Ripple Effect
The COVID-19 pandemic added pressure to already overburdened teams. Extra stressors contributing to burnout include:
- Heavy burdens of work with rapidly changing needs, recommendations and resources.
- Expectation to work outside areas of expertise to support the burden.
- Growing backlogs of elective and non-COVID-19 care.
- Personal risk of being exposed to the virus and exposing their households.
- Work-life conflict between demanding work schedules and expanded personal responsibilities, from older relatives needing extra support to children attending school at home.
Though heightened by the pandemic, these stressors are expressions of deeper problems at the system level. Unless organizations take action, teams will continue to struggle with burnout long after this crisis fades from the headlines.
Burnout: A systems approach
Addressing burnout on a systems level means coordinating many different aspects of the healthcare environment. As NAM puts it, “A systems approach incorporates thorough knowledge of the stakeholders, their goals and activities, the technologies they use, and the environment in which they operate.”4
The graphic below visualizes the functions and aspects of this system to show where organizations have the opportunity to uproot and reduce burnout.
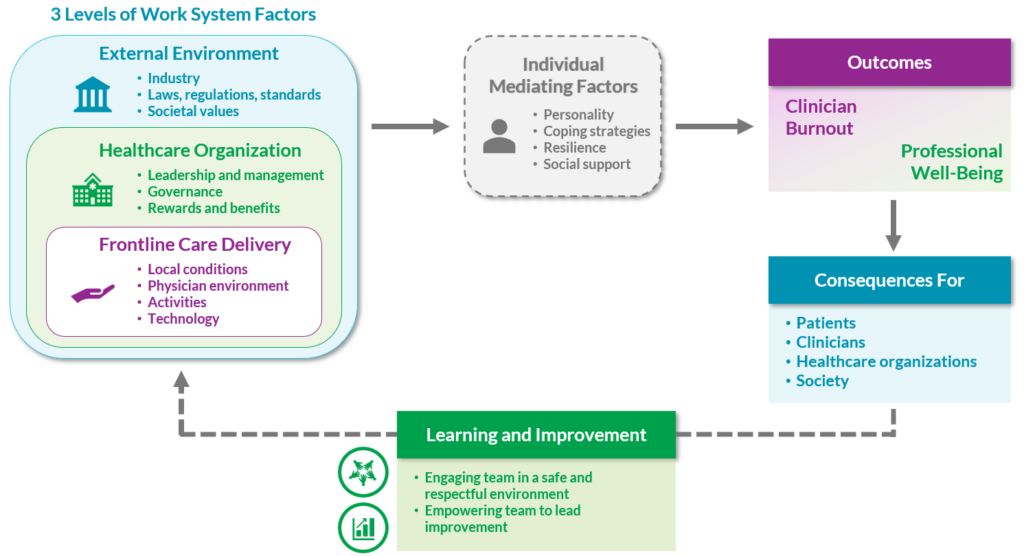
A Systems Model of Clinician Burnout and Professional Well-Being
Adapted from National Academies of Sciences, Engineering, and Medicine 2019. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington, DC: The National Academies Press. https://doi.org/10.17226/25521.
Excessive bureaucratic tasks and other job demands that contribute to burnout fall in the area of “work system factors” (upper left). This area also includes aspects of a job that can diminish burnout, such as:
- Control, flexibility and autonomy at work
- Finding meaning and purpose in work
- Work-life integration
- Organizational culture, professional relationships and support
The key, as depicted at the bottom of the graphic, is for organizations to instill an environment of continual learning and improvement. This fuels the positive work system factors that boost well-being and reduce burnout.
Specifically, NAM’s model recommends engaging teams in a safe and respectful setting and empowering teams to lead change.
Respect and empowerment: Two core pillars to improve engagement
Respect and empowerment are also core principles of the Virginia Mason Production System® (VMPS), the management model used throughout the Virginia Mason Medical Center. We’ve seen firsthand how these principles help reduce burnout and support well-being.
At one Virginia Mason clinic, the turnover rate among medical assistants is one-third the national average (8% compared to 25%). In a 2018 employee survey, 90% of the clinic’s nonclinician staff and 93% of clinicians reported feeling “content” or “engaged.”
Respect and empowerment both come through in the expectations and practices set at the systems level of an organization. And both principles must be cultivated in order to reduce burnout.
1. Respect for People:
Engaging your teams and ensuring a respectful environment
Respect for People informs the way workers at all levels interact, from pointing out mistakes to listening to feedback. Embracing this principle also means creating a structure for respectful interactions, such as giving everyone in a meeting an opportunity to speak and a duty to own, rather than having one person lead and everyone else listen.
In a respectful environment, team members:
- Feel safe to raise concerns without fears of retribution
- Can fully contribute
- Feel heard and encouraged
- Find their work engaging, rewarding and aligned with their personal and professional development goals
Workers who are respected on a daily basis are far less likely to burn out. They feel supported and engaged rather than alone and disconnected. And they feel safe asking for help with problems like long hours and burdensome tasks.
How to do it
Some ways you can approach making improvements with this pillar include:
- Promote personal and professional development: Leaders should help their staff set individual goals that align with team, department, and organization goals. This helps team members see their role and value in the bigger picture.
- Ask for input and feedback: Team members, regardless of their position, should feel safe to share ideas through focused huddles, an idea-sharing process, and leader involvement.
- Talk about it in the open: Leaders and team members can have small-group discussions about the concept of respect and all the ways it can color their work. Use supporting materials like our downloadable poster listing 10 foundational behaviors of respect.
- Participate in training: Host and attend workshops and trainings on diversity, equity, and inclusion (DEI), respect behaviors, empathy, and communication. Encourage and enable everyone, from executives to frontline staff, to participate.

Taking a first step: Facilitating targeted discussions around respect, well-being and burnout can be difficult or uncomfortable even for experienced leaders. We help make this easier with discussion guides and templates — like the Speaking Up to Disrespect activity guide. Use this activity guide to help engage your team in a targeted activity and discussion around respect behaviors.
2. Continuous Improvement:
Empowering your teams to improve their workflows
Continuous improvement directly builds on a culture of respect. Team members are not only encouraged to speak up about problems but also empowered to develop and propose solutions. This means including frontline workers in improvement initiatives, rather than handing down solutions they had no voice in shaping. It also means making improvement part of the daily expectation and habit of work.
This often has the double benefit of improving patient care or experience and improving staff productivity and morale. When workers help solve the problems getting in their way, they eliminate the sources of waste and inefficiency that contribute to feelings of burnout.
It’s vital to find a balance, however. Focusing too much on process improvement can make workers feel stressed and insecure. So this is where respect re-enters the equation: When workers know they are respected, they willingly contribute to improvements and the broader organization.
How to do it
To encourage continuous improvement within your team:
- Train team members: Spread learning on how to lead improvement work with observation, flow mapping, and data collection.
- Sponsor improvement work: Identify specific processes that are tied to team, department, and organizational goals and set aside time and personnel to focus on improving them.
- Develop clear communication flows: Transparency can reduce ambiguity, frustration, and room for error.
- Standardize equipment setup: Reduce waste, misuse, and potential errors — not to mention stress — associated with improper setup.
- Develop clear, easy-to-understand daily huddle dashboards: Team members should always have a sense of who’s in the clinic, who’s working with whom, daily patient demand, and coverage needed.

Taking a first step: Does your team have a way to gather ideas? Use this toolkit to jumpstart your team’s ability to develop a standard way to connect regularly. You’ll learn to collect new ideas and prioritize how to move the best ideas forward.
Burnout isn’t just another problem — it’s THE problem
It can feel like too much to try to implement systems changes while still caring for patients in the aftermath of the pandemic. But burnout isn’t an add-on to the challenges of healthcare management. In many ways, it’s the challenge facing healthcare organizations today.
Burnout increases the difficulty of team member recruitment and retention in an already-cramped environment. And it increases the likelihood of your team members making mistakes that can impact patient well-being.
The good news is that you can support professional well-being in meaningful ways right now, with the tips and tactics shared above. And you don’t have to do it alone. Get in touch to find out how we can help.
“[Training with Virginia Mason Institute] has provided a common language to communicate in. This is extremely important in this crazy time and it allows a non-threatening way for others to identify they need help without necessarily having to ask for it. The daily huddles highlight where the busy areas are for the day and where there may be resources to help. This has led to increased engagement and better collaboration.”
Sara Hebel, MHA Vice President, Ambulatory Operations Pierce Region Franciscan Medical Group Administration
Originally published May 26, 2021, updated March 23, 2022
References
1. Reith TP. Burnout in United States Healthcare Professionals: A Narrative Review. Cureus. 2018;10(12):e3681. Published 2018 Dec 4. doi:10.7759/cureus.3681
2. Zindel, M., K. Cappelucci, H. C. Knight, N. Busis, andC. Alexander. 2019. Clinician Well-Being at VirginiaMason Kirkland Medical Center: A Case Study.NAM Perspectives. Discussion Paper, NationalAcademy of Medicine, Washington, DC. https://doi.org/10.31478/201908c
3. De Hert S. Burnout in Healthcare Workers: Prevalence, Impact and Preventative Strategies. Local Reg Anesth. 2020;13:171-183. Published 2020 Oct 28. doi:10.2147/LRA.S240564
4. National Academies of Sciences, Engineering, and Medicine 2019. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington, DC: The National Academies Press. https://doi.org/10.17226/25521.
Executives and Senior Leaders
Learn more about your role in making sure your team members don’t face increasing burnout and have the support needed to improve their workflows and increase engagement.
Process Improvement and Operational Leaders
You can get started using our free tools mentioned in this article, but if you’re ready for additional training and coaching we encourage you to learn more about our introductory Improving Flow workshop, our Advanced Process Improvement Training intensive program or our Respect for People Training.
Watch the Webinar
Learn about the crucial role leaders have in creating a culture of respect and continuous improvement that engages team members and the strategies you can immediately implement to promote workforce well-being and resilience.