Vaccination Flow 101: Three Fundamentals for Improving Your Vaccine Throughput
We are hearing again and again that now is the time to look back to the fundamentals of process improvement as we face ongoing challenges related to COVID-19. Now is the time to go back to basics and apply them in new ways, whether it’s in your COVID vaccination distribution efforts or with challenges you face in transitioning to a new world of virtual care. Regardless of the specific challenge, it’s crucial you and your team have a strong understanding of your patient demand, Flows of Medicine, and removing waste. We’re proud to see our partners rely on these fundamentals to make strides in their vaccine rollouts, and we’d like to share some key foundational principles of the Virginia Mason Production System® that can help you as you work to bring vaccinations to your team members and community.
1. Understand Your Pace of Work
“Takt” is a German word that means “beat” or “pace” and is calculated by dividing your time available by your expected demand. This calculation will guide the pace of the work and resources needed. Your resources can be extensive and complex but understanding takt time is foundational to be able to meet your customer demand. For a deeper dive into understanding takt time in healthcare, more information can be found here. The key is to be able to have a clear expectation of how much time you can devote to each patient while ensuring you can meet your day’s total demand.

2. Map Your Critical Flows
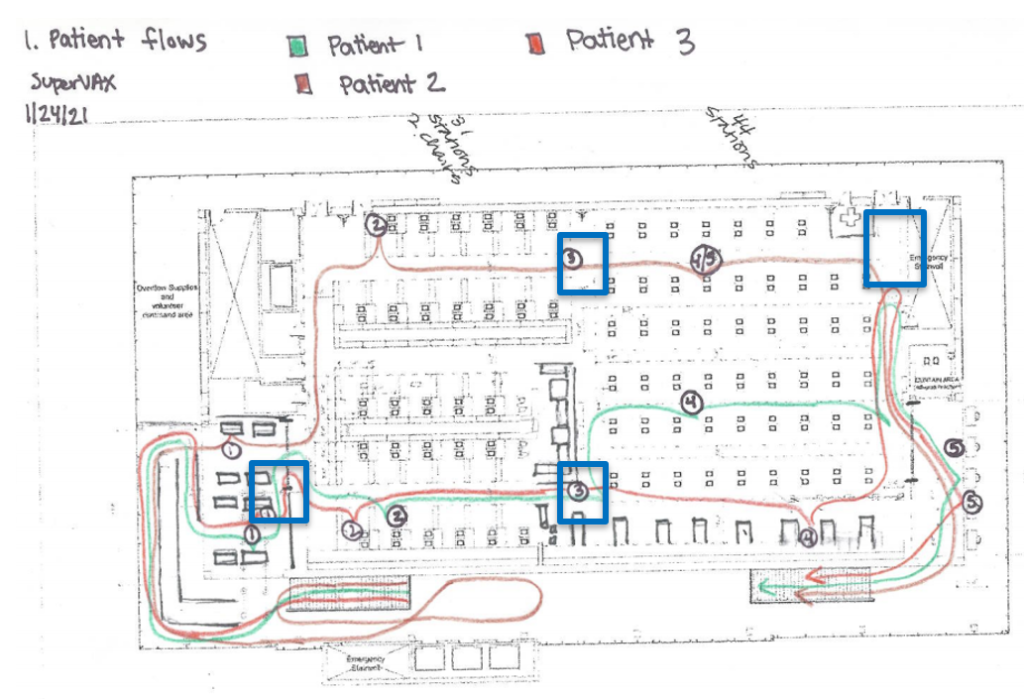
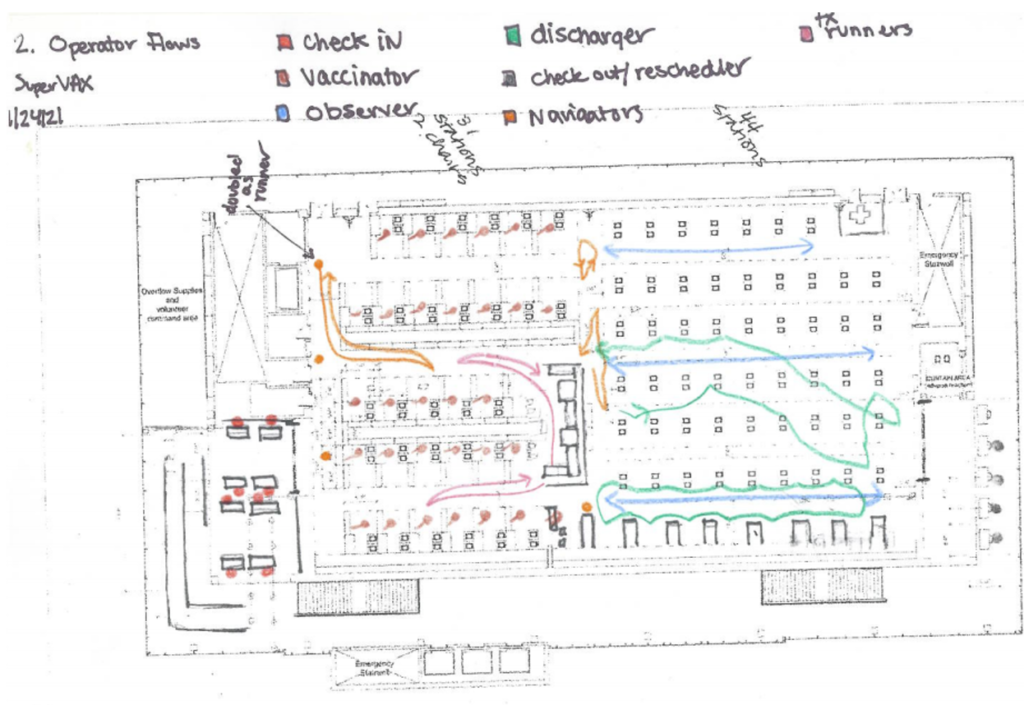
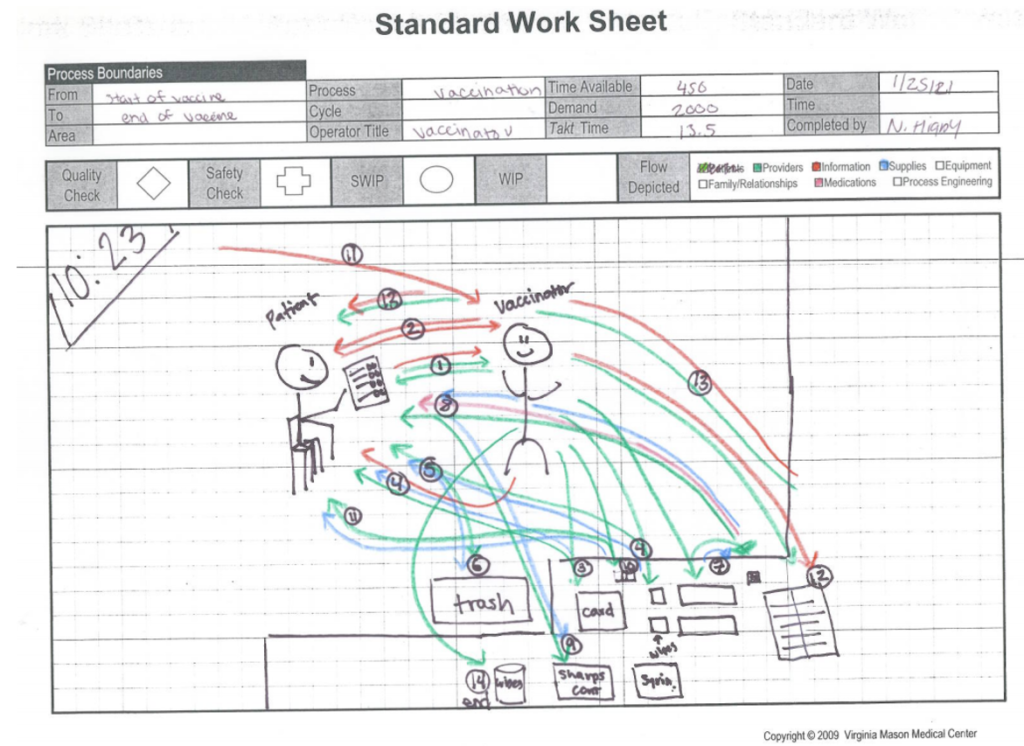
Mapping critical flows allows your team to understand what is working well and what might need improvement. Virginia Mason Institute has identified 8 critical Flows of Medicine to ensure all aspects of the experience are made visual. Mapping flows doesn’t need to be overwhelming, first start with the flow of the patient (first image below). This shows the flow of three patients from check-in (1), through vaccination (2) and observation (3) and concluding with their discharge (4) and exit (5). By mapping the flows, the team was able to identify areas where our 6 feet of physical distancing (blue boxes) were not maintained and when the flows varied between patients. The second image below highlights the flows of the various roles. By mapping the flows of our team members, we were able to see two separate flows of the dischargers; one person is following a standard sequence while the other is not. Insights like this can assist in training and the creation of standards amongst the team. The example in the third image below maps the flows of a single operator, a vaccinator in this case. By mapping the flows, we saw opportunities to improve the arrangement of supplies, resulting in improved ease of work and ergonomics for the vaccinators.
“It was extremely helpful to have our [improvement team] observe and measure timing with the flow of the vaccination process.”
-Kim Capan, Strategic Support Manager, Medical Affairs, University of Maryland St. Joseph Medical Center
3. Create a Team of Waste Detectives
Waste is everywhere and reducing/eliminating it improves the patient experience, improves the team member work environment and will support quality during your vaccination events. Understanding the Seven Wastes to Build a Lean Foundation is a great place to build foundational knowledge of waste with your team. Get creative, ask a patient to identify waste and pass along their observations using the Waste Walk Exercise.
These foundational principles can help you as you continue your work in distributing vaccinations to your team members and community. If you’d like to learn more about how we and client organizations have applied the principles of the Virginia Mason Production System® to our response to COVID-19, visit our Resource page and search COVID to find blogs, case studies and webinars.
If you want to talk through your specific challenge you are facing with your vaccination program, click here to request a complimentary 30-minute consult with one of our Transformation Advisors.
Are you ready to develop advanced process improvement expertise?
Learn more about our virtual intensive certificate program – Advanced Process Improvement Training.
“This course work came in at the perfect time as the topics we covered in class aligned perfectly with a vaccine delivery clinic we created and we used almost every tool taught 100% to deploy something outside of our comfort zone, and it was wildly successful!” – Chuck Hampston, Lean and Process Improvement Coordinator, Memorial Medical Center, Ashland WI